Medical coding is an essential aspect of healthcare. It involves converting medical services, procedures, diagnoses, and symptoms into designated codes. These codes are then used for various purposes, such as billing, insurance claims, and statistical analysis. Accurate coding ensures that information is properly documented and shared among healthcare providers, researchers, and policymakers. In the case of a malignant neoplasm of the left olfactory nerve, understanding the code is crucial for effective treatment and management.
Understanding Medical Coding
Medical coding is a standardized system that helps organize and classify medical information. It simplifies the communication between healthcare professionals, insurance companies, and regulatory entities by providing a universal language. Each medical code represents a specific diagnosis, procedure, symptom, or medication, allowing for precise documentation and better patient care.
Medical coding is an essential component of the healthcare industry, ensuring that accurate and detailed information is recorded and transmitted. It serves as a bridge between healthcare providers and insurance companies, facilitating the reimbursement process. By using standardized codes, healthcare professionals can effectively communicate the nature of a patient’s condition, the procedures performed, and the medications prescribed.
Moreover, medical coding plays a crucial role in research and data analysis. By accurately coding medical information, researchers can analyze health trends, evaluate treatment outcomes, and identify patterns in disease prevalence. This data is invaluable in shaping healthcare policies, designing public health initiatives, and improving overall patient care.
The Importance of Accurate Medical Coding
Accurate medical coding plays a significant role in the healthcare industry. It ensures proper reimbursement for healthcare providers and facilities by correctly documenting the services rendered. Moreover, accurate coding contributes to improved patient care as it helps in identifying medical conditions, monitoring health trends, and evaluating treatment outcomes. Consequently, healthcare policies, research studies, and population health initiatives heavily rely on accurate coding data.
When medical coding is inaccurate or incomplete, it can lead to various issues. For healthcare providers, incorrect coding can result in delayed or denied payments from insurance companies, leading to financial strain. Inaccurate coding can also impact patient care, as it may result in incorrect diagnoses, inappropriate treatments, or missed opportunities for preventive care.
To ensure accuracy in medical coding, healthcare professionals undergo extensive training and certification. They must stay updated with the latest coding guidelines and regulations to accurately document and code medical information. Additionally, healthcare organizations often have coding specialists or teams dedicated to reviewing and auditing coding practices to maintain compliance and accuracy.
Basics of Medical Coding
Medical coding is primarily based on two coding systems: International Classification of Diseases (ICD) for diagnoses and Current Procedural Terminology (CPT) for procedures. These systems are regularly updated to reflect advancements in medical science and technology. For the code of a malignant neoplasm of the left olfactory nerve, the ICD-10 coding system is used. This system provides a detailed and comprehensive framework for classifying diseases, including cancerous growths like malignant neoplasms.
The ICD coding system is used worldwide and is continuously expanded and revised to accommodate new diseases, treatments, and medical knowledge. It provides a standardized way to classify and code diagnoses, enabling healthcare professionals to accurately communicate a patient’s condition. The ICD-10 coding system, in particular, allows for greater specificity, with codes that provide detailed information about the location, severity, and type of disease.
On the other hand, the CPT coding system focuses on procedures and services provided by healthcare professionals. It provides a standardized set of codes that describe medical, surgical, and diagnostic procedures. These codes help in accurately documenting the services rendered, ensuring proper billing and reimbursement.
Both the ICD and CPT coding systems are essential tools in medical coding, enabling healthcare professionals to accurately document and communicate medical information. By using these systems, healthcare providers can ensure that the appropriate codes are assigned, leading to accurate billing, improved patient care, and reliable data for research and analysis.
Defining Malignant Neoplasm
Malignant neoplasms, commonly known as cancer, are abnormal and uncontrolled growths of cells. They invade nearby tissues and have the potential to spread to other parts of the body. This uncontrolled growth occurs when the normal mechanisms that regulate cell division and growth are disrupted, leading to the formation of a tumor. Malignant neoplasms can arise from various types of cells in the body, including epithelial cells, connective tissue cells, and blood cells.
When a malignant neoplasm develops, it can cause a range of symptoms depending on its location and size. Some common symptoms include pain, fatigue, weight loss, and changes in bodily functions. These symptoms can be attributed to the tumor’s interference with the normal functioning of organs and systems.
Characteristics of Malignant Neoplasms
Malignant neoplasms are characterized by their ability to invade nearby tissues and metastasize to distant sites. This invasive behavior sets them apart from benign neoplasms, which are usually localized and do not invade surrounding tissues. The ability of malignant neoplasms to invade nearby tissues is facilitated by the alteration of certain genes and proteins involved in cell adhesion and migration.
Metastasis, the spread of malignant neoplasms to distant sites, is a complex process involving the detachment of cancer cells from the primary tumor, their entry into blood or lymphatic vessels, and their subsequent colonization in distant organs or tissues. This ability to metastasize makes malignant neoplasms particularly dangerous, as it allows them to establish secondary tumors in different parts of the body.
Differentiating Between Benign and Malignant Neoplasms
Distinguishing between benign and malignant neoplasms is essential for accurate diagnosis and appropriate treatment. While benign neoplasms are typically localized and encapsulated, malignant neoplasms infiltrate surrounding tissues and have the potential to spread. This distinction is crucial because the treatment approaches for benign and malignant neoplasms differ significantly.
Diagnostic procedures play a vital role in determining whether a neoplasm is benign or malignant. Imaging tests, such as X-rays, computed tomography (CT) scans, and magnetic resonance imaging (MRI), can provide valuable information about the size, location, and extent of the tumor. Biopsies, which involve the removal of a small sample of tissue for examination, allow pathologists to assess the cellular characteristics of the neoplasm.
Histopathological examinations, which involve the microscopic examination of tissue samples, are particularly useful in differentiating between benign and malignant neoplasms. Pathologists analyze the cellular features, growth patterns, and presence of certain markers to determine the neoplasm’s nature. These examinations provide crucial information that guides the treatment decisions and prognosis for patients.
In conclusion, malignant neoplasms are aggressive and potentially life-threatening tumors that invade nearby tissues and have the ability to spread to distant sites. Understanding the characteristics of malignant neoplasms and differentiating them from benign neoplasms is crucial for effective diagnosis and treatment. Through advancements in diagnostic procedures and research, healthcare professionals continue to improve their understanding of malignant neoplasms, leading to more targeted and effective treatments for patients.
The Olfactory Nerve Explained
The olfactory nerve, also known as the first cranial nerve, is responsible for the sense of smell. It transmits sensory signals from the nose to the brain, allowing us to detect and identify various scents. The olfactory nerve plays a vital role in our daily lives, influencing our perception of taste, emotions, and memory.
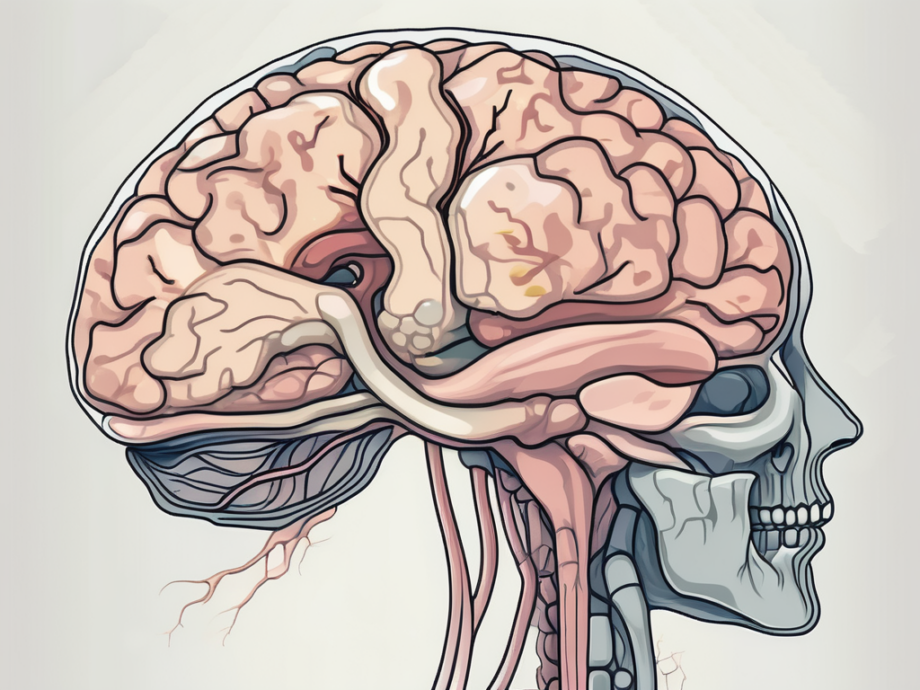
Anatomy of the Olfactory Nerve
The olfactory nerve originates from specialized cells within the nasal cavity called olfactory receptor cells. These cells contain receptors that detect odor molecules in the air. When we inhale, these receptors bind to the odor molecules, initiating a cascade of events that ultimately leads to the transmission of signals along the olfactory nerve.
From the olfactory receptor cells, the nerve fibers of the olfactory nerve travel through tiny openings in the skull, known as cribriform plates. These plates are located at the roof of the nasal cavity, allowing the nerve fibers to pass through and connect to the olfactory bulb, which is located at the base of the brain.
The olfactory bulb is a specialized structure that acts as a relay station for the olfactory nerve. It receives the sensory information from the nerve fibers and then sends it to different brain regions for processing and interpretation. This complex network of connections allows us to make sense of the various smells we encounter in our environment.
Functions of the Olfactory Nerve
The olfactory nerve allows us to detect and distinguish various odors. It contributes to our ability to fully experience and enjoy food, as the sense of smell greatly influences our perception of taste. For example, when we have a stuffy nose due to a cold, our ability to taste food is often diminished because the olfactory nerve is not able to transmit the necessary sensory signals to the brain.
Moreover, the olfactory nerve is closely linked to our emotions and memory. Certain smells can evoke strong emotional responses and trigger vivid memories. This phenomenon is known as the “Proustian effect,” named after the French writer Marcel Proust, who famously described how a simple smell could transport him back to his childhood memories.
Additionally, the olfactory nerve plays a crucial role in our sense of danger. It can alert us to potentially harmful substances or environments by detecting certain chemical cues in the air. This ability to detect and recognize dangerous smells is essential for our survival and well-being.
In conclusion, the olfactory nerve is a remarkable structure that allows us to experience and navigate the world through our sense of smell. Its intricate anatomy and functions contribute to our overall sensory perception, emotional experiences, and memory formation. Understanding the olfactory nerve helps us appreciate the complexity of our olfactory system and the important role it plays in our daily lives.
Malignant Neoplasm of the Left Olfactory Nerve
A malignant neoplasm of the left olfactory nerve refers to a cancerous growth in the left olfactory nerve. This condition is relatively rare but can have significant implications for the affected individual’s health and wellbeing.
The olfactory nerve, also known as the first cranial nerve, plays a crucial role in our sense of smell. It is responsible for transmitting signals from the nasal cavity to the brain, allowing us to perceive and distinguish various odors. However, when a malignant neoplasm develops in this nerve, it can disrupt its normal functioning and lead to a range of symptoms and complications.
Symptoms and Diagnosis
The symptoms of a malignant neoplasm of the left olfactory nerve can vary depending on various factors, including the size and location of the tumor. Common symptoms may include persistent nasal congestion, changes in smell perception, frequent nosebleeds, facial pain or numbness, and vision disturbances.
Patients with this condition often experience persistent nasal congestion, which can be accompanied by difficulty breathing through the affected nostril. The changes in smell perception can range from a diminished sense of smell to a complete loss of smell, known as anosmia. These olfactory disturbances can have a significant impact on the patient’s quality of life, affecting their ability to enjoy food, detect danger, or appreciate pleasant scents.
In some cases, the tumor may cause frequent nosebleeds, which can be alarming and may require medical intervention to control the bleeding. Facial pain or numbness can also occur due to the tumor’s compression of nearby structures, such as the facial nerve. Additionally, vision disturbances may arise if the tumor extends into the adjacent areas, affecting the optic nerve or other visual pathways.
Diagnosis typically involves a combination of imaging tests, such as magnetic resonance imaging (MRI), and biopsies to confirm the presence of a malignant neoplasm. MRI scans can provide detailed images of the tumor, allowing healthcare professionals to assess its size, location, and potential involvement of surrounding structures. Biopsies, on the other hand, involve the removal of a small tissue sample from the tumor for laboratory analysis, providing a definitive diagnosis.
Treatment Options and Prognosis
The treatment for a malignant neoplasm of the left olfactory nerve may involve a multidisciplinary approach, including surgery, radiation therapy, and chemotherapy. The specific treatment plan depends on factors such as the stage of the tumor, the patient’s overall health, and their individual preferences.
Surgery is often the primary treatment modality for localized tumors. The goal is to remove as much of the tumor as possible while preserving the surrounding healthy tissues and structures. In some cases, a complete resection may not be feasible due to the tumor’s location or size, and a partial removal or debulking procedure may be performed to alleviate symptoms and improve the patient’s quality of life.
Radiation therapy, which involves the use of high-energy beams to target and destroy cancer cells, may be recommended as an adjunct to surgery or as the primary treatment for inoperable tumors. This treatment modality aims to shrink the tumor, control its growth, and relieve symptoms. Chemotherapy, on the other hand, utilizes powerful drugs to kill cancer cells throughout the body and may be used in cases where the tumor has spread beyond the olfactory nerve.
Prognosis can vary and is influenced by several factors, including the tumor’s size, location, and response to treatment. Early detection and intervention generally offer a better prognosis, as they allow for more effective treatment and management of the condition. Regular follow-up appointments and surveillance are essential to monitor the patient’s progress, detect any recurrence or metastasis, and provide appropriate supportive care.
The Coding Process for Malignant Neoplasm of the Left Olfactory Nerve
The coding process for a malignant neoplasm of the left olfactory nerve follows specific guidelines to ensure accuracy and consistency in medical documentation.
When it comes to coding a malignant neoplasm of the left olfactory nerve, healthcare professionals rely on the use of ICD-10 codes. These codes play a crucial role in classifying and coding specific diseases, providing detailed information about the condition, including the site of the tumor, its nature, and its stage. By utilizing ICD-10 codes effectively, healthcare providers, insurance companies, and researchers can accurately identify and track specific diseases, such as a malignant neoplasm of the left olfactory nerve.
The Role of ICD-10 Codes
ICD-10 codes are an essential tool in the world of medical coding. These codes serve as a standardized system for classifying diseases and medical conditions, ensuring consistency and accuracy in medical documentation. Specifically, when it comes to a malignant neoplasm of the left olfactory nerve, ICD-10 codes provide healthcare professionals with a comprehensive framework to describe the condition in a precise and detailed manner.
By assigning the appropriate ICD-10 codes, healthcare providers can convey vital information about the tumor’s location, its characteristics, and its stage. This level of specificity is crucial for effective communication among healthcare professionals, as well as for research purposes. Additionally, insurance companies rely on these codes to determine coverage and reimbursement for medical services related to a malignant neoplasm of the left olfactory nerve.
Steps in Medical Coding
The coding process for a malignant neoplasm of the left olfactory nerve involves several important steps. Firstly, the medical coder carefully reviews the patient’s medical records, including diagnostic reports, imaging results, and surgical notes. This thorough examination ensures that the coder has a comprehensive understanding of the patient’s condition and the necessary information to assign accurate codes.
Once the medical coder has gathered all the relevant information, they proceed to assign the appropriate ICD-10 codes. This step requires a deep understanding of the coding guidelines and a thorough knowledge of medical and anatomical terminology related to the condition. By accurately selecting the right codes, the medical coder ensures that the documentation reflects the true nature of the malignant neoplasm of the left olfactory nerve.
It is worth noting that medical coders play a vital role in the healthcare system, as their expertise ensures that accurate and detailed information is recorded. This information is not only crucial for patient care but also for research purposes, as it allows for the analysis of trends and outcomes related to a malignant neoplasm of the left olfactory nerve.
In conclusion, the coding process for a malignant neoplasm of the left olfactory nerve involves the use of ICD-10 codes, which provide detailed information about the condition. Medical coders play a crucial role in accurately assigning these codes based on the specific details of the tumor. Their expertise ensures that healthcare providers, insurance companies, and researchers have access to accurate and consistent information for effective patient care and analysis.
Implications of Coding in Healthcare
The coding of a malignant neoplasm of the left olfactory nerve has far-reaching implications in the healthcare industry, including patient care, policy decisions, and medical research.
When it comes to patient care, accurate coding is of utmost importance. It ensures that healthcare providers have access to complete and precise information about a patient’s medical condition. This information facilitates appropriate treatment plans, adherence to clinical guidelines, and proactive care management. For example, if a patient is diagnosed with a malignant neoplasm of the left olfactory nerve, accurate coding allows healthcare professionals to tailor their treatment approach to address the specific challenges associated with this condition. It also helps in identifying potential complications or comorbidities that may require additional attention.
Moreover, accurate coding contributes to effective communication among healthcare professionals. It serves as a universal language that ensures continuity and coordination of care. When different healthcare providers, such as doctors, nurses, and specialists, are involved in a patient’s treatment, accurate coding enables seamless sharing of information. This leads to improved collaboration and reduces the risk of errors or misunderstandings that could negatively impact patient care.
Influence on Healthcare Policies and Research
The impact of coding data extends beyond individual patient care. It plays a crucial role in shaping healthcare policies and regulations. Government agencies, insurance companies, and research institutions rely on accurate coding information for statistical analysis, health surveillance, and resource allocation.
For instance, when analyzing coding data related to malignant neoplasms, policymakers can gain insights into the prevalence and distribution of these conditions. This information helps in identifying areas where additional resources or preventive measures may be needed. It also aids in evaluating the effectiveness of current healthcare policies and making informed decisions regarding their improvement or modification.
In addition, coding data is invaluable for medical research. Researchers can utilize coding information to identify trends, risks, and potential areas for improvement in cancer prevention, diagnosis, and treatment. By analyzing coding data, they can identify patterns in the occurrence of malignant neoplasms of the left olfactory nerve and explore potential factors contributing to their development. This knowledge can lead to the development of new treatment strategies, diagnostic techniques, or preventive measures.
In conclusion, understanding the code for a malignant neoplasm of the left olfactory nerve is essential for effective treatment and management. Medical coding serves as a universal language that ensures accurate documentation, efficient communication, and improved patient care. By accurately coding a malignant neoplasm, healthcare providers can contribute to better treatment outcomes, patient safety, and advancements in healthcare policies and research.